Stress Fractures
Stress fractures are tiny cracks in the bone, which occur when muscles are overexerted and lose the ability to absorb shock, which is then transferred to the bone. People who develop stress fractures are usually those engaged in repetitive weight-bearing activities, such as running, tennis, basketball, and gymnastics. Having flat feet, rigid arches, or osteoporosis will increase your risk of a stress fracture, which typically occurs in the lower leg or foot. To prevent such injury, build up the intensity and duration of your exercise routine gradually so your muscles have time to strengthen. Symptoms include pain that increases with time and is still painful after a few days. The pain increases with activity, and there may or may not be swelling. You should go to a doctor if the pain doesn’t go away after 2 days of rest.
Sprains
A sprain occurs when a ligament (the fibrous tissue that connects bones) is overstretched or torn, but there is no dislocation or fracture. The sprained joint will cause immediate pain, swelling, bruising, and warmth at the injured site. As the sprain heals, the damaged ligaments and connective tissue will be replaced by new fibrous tissue that is stronger, but not as flexible. This is why it’s important to move and stretch the injured site during the healing process, as long as it doesn’t cause pain. The joint may not fully recover for many weeks.
To treat sprains, follow R.I.C.E. (described below), and make sure ankle sprains are elevated above heart level even during sleep. Standing or dangling the leg can lead to more swelling, throbbing, and pain. Do not treat acute sprains with heat, only ice.
The best pain reliever to take right after injury is Ibuprofen because it is also anti-inflammatory (decreases swelling). Acetaminophen (Tylenol) is not an anti-inflammatory and Aspirin will increase internal bleeding if taken within 24 hours of the injury. Always consult a physician for information on use of medications. Crutches are useful if the leg cannot bear weight fully, but early walking is important to prevent tightening of the tendons that connect muscles to bones.
Strains
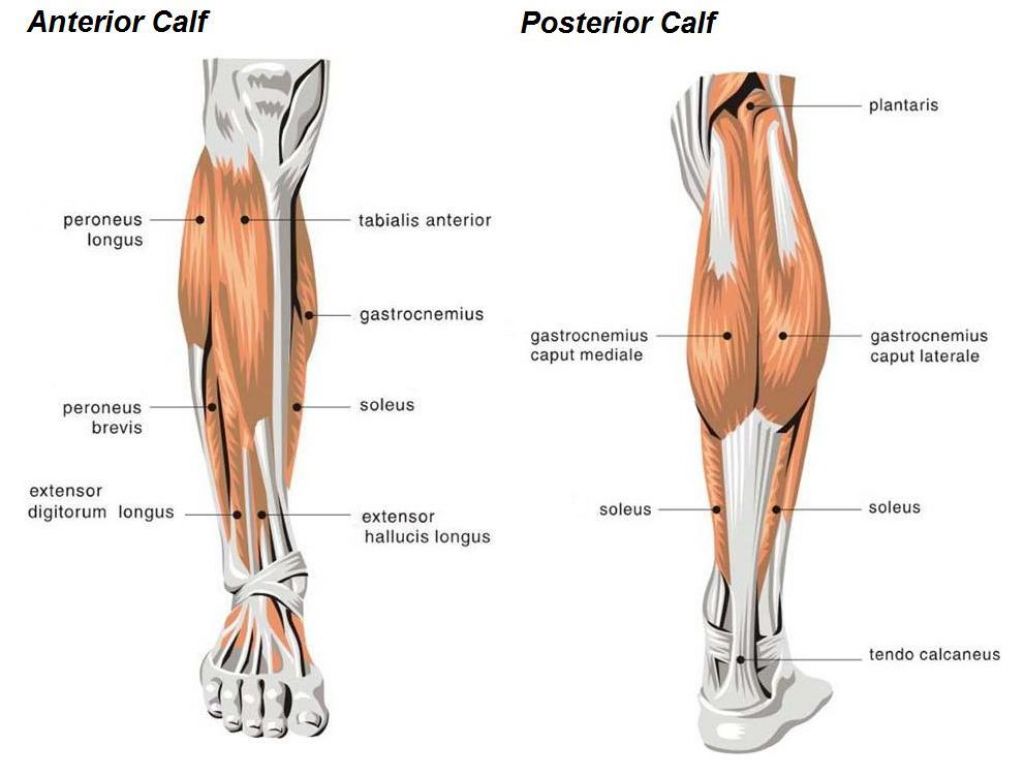
Strains are often the result of overuse or injury, when muscles or tendons are overstretched or overexerted. While sprains concern ligaments, strains affect tendons, the tissue that connects muscles to bones. Strains cause pain, tenderness, swelling, and bruising at the injured site. Because sprains and strains affect different types of tissue, you can have both types of injury at the same time. For example, an ankle sprain and a strain of the Achilles tendon.
Tendonitis (also spelled “tendinitis”)
Tendonitis is any inflammation or irritation of a tendon, which connects muscles to bone. The condition causes pain, tenderness, and stiffness near a joint, usually around the shoulders, elbows, and knees, and is commonly the result of injury or overuse. The pain of tendonitis is aggravated by movement, so rest, ice, and pain medication is usually the best treatment. In order to avoid tendonitis, don’t participate in activities that place abnormal amounts of stress on your tendons, such as running uphill. Also, try cross-training to limit and spread out high-impact workouts, such as running.
Treating Sprains, Strains and other Sports Injuries
If the injury does not appear serious, stop what you’re doing and use R.I.C.E.:
- Rest the injured area as much as possible for 24 to 48 hours.
- Ice the injured area as soon as possible for 20 minutes on and 20 minutes off. After a couple hours you can reduce icing to 20 minutes 4 times a day.
- Compression. Apply an elastic bandage to the area to control movement, but loosen it if you feel numbness, tingling, or increased pain.
- Elevation. Raise the injured area above heart level.
Full return to activity should be avoided until full range of motion no longer causes pain.