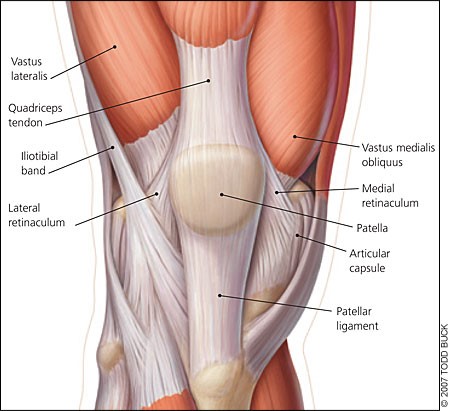
Patello-femoral pain syndrome is an inflammation to the front of the knee joint caused by the patella (knee cap) not tracking properly over the distal femur (thigh bone at the knee). The patella normally rides in a groove on the femur. The patella is like a fulcrum, it gives leverage to the big muscles on the front of the thigh. These thigh muscles are called the quadriceps because they consist of four muscles
With patello-femoral syndrome (PFS), you get an imbalance in these muscles—usually the lateral or outside muscle overpowers the inner medial muscle, and this pulls the patella out of its normal groove. When the patella doesn’t track properly, it causes pain under the patella. PFS can have multiple causes, which can include foot problems, such as foot pronation, weak lateral hip muscles, genu valgum (knock-kneed), and a larger Q-angle (the angle from the front hip to middle of the knee cap). These can all affect the biomechanics of the patello-femoral joint. When experiencing these problems with your knee, it’s important to find ways not to keep it irritated.
Occasionally, the injuries start with a clear-cut onset, like stepping in a hole or falling on your knee. Usually, though, it feels like it comes out of nowhere. This means that you’ve been gradually creating the injury over a longer period of time like a few days or weeks. Something that you do during the day sets it off, but it’s commonly very hard to figure out was exactly is the aggravating activity. Nonetheless, you’ve overdone it. Try not to worry if you can’t figure out exactly why your knee got sore. That may not be necessary to determine in order to get better. The more often you make your knee sore, the longer it will take to get better.
The inflammation seldom builds up to a level where it keeps you in bed, so it’s tempting to keep up and about on it. This may keep it stirred up. Try to avoid all the activities that make it sore, i.e., sitting with your knee bent for a long time, walking a lot, going up and down stairs, or exercising. While it doesn’t cause more damage, it does keep the inflammation from going away. You may find it helpful to sit with your knee straight or get up and move around occasionally. Also, try stairs one step at a time using your uninjured leg. These knee injuries can be very stubborn before they get better. The sooner you stop aggravating it, the sooner you can get back to the activities you like.